First, Do No Harm
The WPATH files evidence the impossibility of obtaining informed consent from youth
The World Professional Association for Transgender Health (“WPATH”) has proclaimed itself as the global authority on transgender health care and has always asserted that its standards for gender-affirming care practices are evidence-based. But with the leak of the WPATH Files to independent journalist Michael Schellenberger, one truth has come to light: youth “gender-affirming care” is not based on evidence.
Though unsurprising to many who have followed the systematic evidence reviews of youth gender medicine in European countries like Finland and the UK, the WPATH Files leak confirms that youth gender-affirming care is devoid of scientific evidence. Gender practitioners, under the guise of providing “lifesaving” care, have endorsed the performance of pseudoscientific medical experiments on children, adolescents, and vulnerable adults, and convinced premier medical organizations that WPATH standards should remain the gold standard. However, WPATH’s internal discussions—leaked by whistleblower(s)—reveal that those same-gender practitioners, including mental health experts, endocrinologists, plastic surgeons, etc., are often guessing at methods of treatment and are intentionally violating medical ethics to treat patients. These unregulated experiments come at the cost of treating young children and mentally ill patients (with schizophrenia and other debilitating mental illnesses) with permanent medical interventions that will, at a minimum, make them life-long patients.
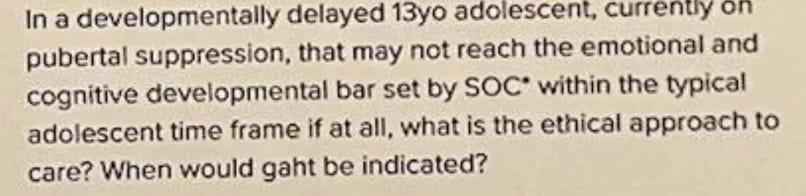
But, as an attorney who works on high-stakes personal injury and medical malpractice cases, I was most interested in the practitioners’ acknowledgment that it is fundamentally impossible to obtain true informed consent from vulnerable patients, particularly children and young adults, for these irreversible interventions which may leave them sterile, without functional genitals, and unable to ever achieve orgasm. In the WPATH Files, one WPATH member states: “[i]t's out of their developmental range sometimes to understand the extent to which some of these medical interventions are impacting them,” and another casually mentions, “We try to talk about it, but most of the kids are nowhere in any kind of a brain space to really, really, really talk about it seriously.” An endocrinologist explains, “I think the thing you have to remember about kids is that we're often explaining these sorts of things to people who haven't even had biology in high school yet.”
These admissions only scratch the surface of the medical, legal, and ethical issues that these gender-affirming treatments create.
From a legal perspective, informed consent is a vital component of medical care. The idea of obtaining true informed consent requires a physician to discuss the treatment plan with a patient and describe the material risks, benefits, and alternatives to care. Informed consent is not always satisfied by signing off a standardized form that describes general risks; instead, it is intended to be a discussion that allows a patient to fully appreciate the effect of his or her decision. In practice, the legal impact—and potential for medical malpractice—exists when a patient can show that a physician did not fully disclose all reasonably foreseeable risks of a treatment, and that the patient received an injury that was measurably greater than if the patient had been fully informed and refused consent.
Another informed consent issue arises if the patient does not have the capacity to consent. The default rule is that every human of adult years and sound mind has the right to determine what shall be done with their body. However, if the patient has a developmental disability or mental illness, or is otherwise of unsound mind, he or she may not have the capacity to consent. Further, coerced consent— “would you rather have a live daughter or a dead son?”—is involuntary consent and exposes physicians to claims of medical malpractice.
In many cases where practitioners are providing gender-affirming treatments, it becomes clear that young people who don’t understand biology are not able to meaningfully consent to experimental care that often imperils their fertility. In other cases, depending on the facts, individuals with severe mental health conditions may also be unable to consent to such permanent, irreversible interventions. Or, where the physicians themselves are not wholly aware of the material risks of an experimental treatment (e.g., from page 18 of the WPATH Files, “WPATH President Bowers admitted in the forum that the effect of puberty blockers on fertility and ‘the onset of orgasmic response’ is not yet fully understood”) or are grossly miseducated about the reality of certain treatments (e.g., “For AFAB persons, pubertal blockade prior to puberty is fully reversible and can offer the significant likelihood of avoiding later surgeries such as top surgery”), any attempt at obtaining informed consent fails because the physicians cannot sufficiently inform patients regarding the effects of treatment.
The WPATH Files provide evidence that many gender practitioners either believe in a questionable-at-best rate of regret declared by activists, or because of ideological priors, are unable to acknowledge the existence of detransitioners altogether. Page 71 of the files states, “acknowledgment that de-transition exists to even a minor extent is considered off limits for many in our community.” Failure to inform patients of the growing rate of regret in individuals receiving various gender-affirming care also violates the principles of informed consent.
The meager “studies” activists cite to demonstrate that detransition or regret is not common amongst patients can easily be dismissed. Detransition and regret rates have not yet been studied thoroughly or reliably, as many studies suffer from limitations of inadequate follow-up for various reasons. Rates of detransition are often skewed, as individuals who claim to have no regret are the same individuals who continue to show up for treatments. Detransitioners, on the other hand, often stop seeing their original gender treatment providers, knowing those clinics will not assist them in their detransition. For example, when presented with the case of an angry 17-year-old patient engaging in detransition and voicing concern over their treatment, a therapist offered the following:
The WPATH Files leak further supports that the experience of a detransitioner is met with disbelief or entirely dismissed as a valid experience.
And, with the 2024 release of a Finnish study concluding that “[c]linical gender dysphoria does not appear to be predictive of all-cause nor suicide mortality when psychiatric treatment history is accounted for,” it has become ever more apparent that the oft-repeated claim that youth gender treatments prevent suicide is false. Though gender activists have repeatedly called for increased accessibility for gender-affirming care to continue to save lives, this Finnish study flips that exact reason on its head. Proper scientific studies continue to poke holes (and sometimes gaping pits) in the so-called evidence-based practice of gender medicine. It appears the credibility of such gender practitioners shall only continue to dwindle, as the legitimate scientific research reveals no change in suicide rates for those receiving gender affirming care to treat gender dysphoria.
Yetin spite of these textbook failures to obtain informed consent, the WPATH Files reveal that gender practitioners continue to encourage themselves and others to surgically and hormonally experiment with children and usher them down the path of irreversible gender treatments.
But given the status quo of statute of limitation laws, there will be no justice for the many victims of youth gender medicine. The statute of limitations for medical malpractice in most jurisdictions generally ranges from 2-4 years, with some jurisdictions allowing extensions based on the discovery rule. In most cases, however, young adults often do not realize that they’ve been unnecessarily harmed by gender-affirming care until five or more years after the last medical intervention. This unfortunate timeline protects physicians and hospitals from lawsuits and leaves the victims of gender-affirming care without recourse. One of the most sensible solutions would be to pass legislation that extends the statute of limitations for medical negligence related to gender-affirming care. Enabling more medical malpractice lawsuits would not only provide justice for victims in the form of financial compensation for the egregious and irreparable harm done to patients, but would also promote increased oversight of the unethical, pseudoscientific practices occurring within hospital walls across America. Some states have already started this reform, with numerous others hopefully following suit.
The WPATH Files are crucial evidence that proves youth “gender-affirming care” is the great medical atrocity of our time, on par with (or perhaps worse than) the 20th Century’s eugenics-motivated involuntary sterilization of those deemed inferior and the frontal orbital lobotomy. WPATH physicians have abdicated their responsibility to “first, do no harm.” Sadly, we are once again reminded that well-meaning medical doctors are not immune from being swept up in the passion of a mass movement or being lured by the financial windfall from these expensive surgeries, consequently forsaking their sacred duty to practice ethical, scientific medicine. It is time for medical doctors who have lost their way to be held accountable.
We welcome you to share your thoughts on this piece in the comments below. Click here to view our comment section moderation policy.
The opinions expressed here do not necessarily reflect those of the Foundation Against Intolerance & Racism or its employees.
In keeping with our mission to promote a common culture of fairness, understanding, and humanity, we are committed to including a diversity of voices and encouraging compassionate and good-faith discourse.
We are actively seeking other perspectives on this topic and others. If you’d like to join the conversation, please send drafts to submissions@fairforall.org.





"I am not a princess anymore. I am a monkey." - my daughter.
When she identified as a non-princess monkey I concluded that she was a 3-year old. It is okay for kids to act like kids and get treated like kids (and adults to act like adults).
Something that I have not yet seen covered in the files is a discussion of “preserved fertility”. I am a parent of two IVF children. To preserve fertility in a young girl of say 13, the doctor would first have to shoot them up with strong hormones to induce a mass production of viable eggs, then harvest and freeze them. If this goes well, they may get a dozen eggs and maybe 8 will the viable. Once they have been frozen and they are then thawed at a later date, viability has been reduced and whether or not they can be successfully fertilized is a whole other issue.
The process of doing this is painful to say the least and it can be life threatening if the mother becomes hyperstimulated. The average 13 year old does not comprehend do I want to have kids, let alone the ramifications of hyper stimulation.